Bilateral adrenal hemorrhage in the Complicated Post-operative Period of Colonic Surgery
Beatriz Cros Montalbán*, Jorge García Egea, Ana Nogués Pevidal, Issa Talal El-Abur, Carlos Yánez Benítez, José Fernando Trebollé, Paola Gracia Gimeno, Juan Luis Blas Laína
Hospital Royo Villanova, Zaragoza, Spain
Abstract
Adrenal hemorrhage is a rare complication that can compromise patient survival. We present the case of a 74-year-old man who, in the complicated post-operative period of a subtotal colectomy for transverse colon adenocarcinoma adjacent to the splenic angle, had significant asthenia, hypotension, and hyponatremia on the blood test. Abdominal CT scan and basal cortisol in blood were performed, compatible with bilateral adrenal hemorrhage and adrenal insufficiency. Treatment with intravenous corticoid was initiated, with the recovery of blood pressure and natremia. The clinical manifestations of bilateral adrenal hemorrhage secondary to intra-abdominal sepsis are usually imperceptible and attributed to other post-operative problems, making it difficult to reach a diagnosis, although early detection makes it possible to treat satisfactorily.
Introduction
Adrenal hemorrhage is a rare complication that can compromise patient survival. The clinical manifestations are often non-specific. Early diagnosis is a key to favourable outcome1-3.
Case presentation
74-year-old male with a history of hypertension and hypothyroidism. After a positive fecal occult blood test, he was diagnosed with adenocarcinoma of the transverse colon adjacent to the splenic angle. Presented at the Digestive Tumors Committee, the patient was intervened in a programmed way by performing subtotal colectomy by laparoscopy (Pathology report: adenocarcinoma of the colon stage pT3N1a(1/61)M0), without incidents and with antithrombotic prophylaxis (subcutaneous sodium bemiparin 3500 UI (according to protocol) every 24 hours).
On the second post-operative day, on examination, he was hypotensive (84/54 mmHg), tachycardic (107 beats per minute), his respiratory rate was 23 breaths per minute, he had 97% oxyhemoglobin saturation on room air and he was afebrile (36.8ºC). Physical examination revealed a mild abdominal distension without abdominal pain. Relevant blood tests showed acute kidney injury, leukopenia and coagulopathy: Creatinine 1,80 mg/dl (normal range, 0.0-1,20), Urea 52 mg/dL (normal range, 16-48), Sodium 136 mEq/L (normal range 136.0-145.0), Potassium 3.9 mEq/L (normal range, 3.5-5.1) Lactic acid 5.5 mmol/L (normal range 0.9-1.9), C-reactive protein 31.59 mg/dL (normal range 0.10-0.50), Procalcitonin 5.63 ng/mL, White cell count x 109/L 1.8 x109/L (normal range 3.6-10.5) , Neutrophils % 86.8% (normal range 40.0-70.0), Hemoglobine 11.7 g/dL (normal range 13.0-18.0), Hematocrit 34.1% (normal range 39.0-52.0), Platelets 141 x109/L (normal range 125-450), Prothrombin activity 68% (normal range 81-140), International normalized ratio 1.39 (normal range 0.8-1.2). An urgent computed tomography scan of the patient´s abdomen and pelvis revealed pneumoperitoneum and the presence of free liquid in the abdominal cavity.
A laparoscopy was performed aiming purulent diffuse peritonitis (fluid samples are taken for culture) secondary to small-bowel ischemia adjacent to the ileocolic anastomosis, and resection of the anastomosis, terminal ileostomy in the right iliac fossa and closure of the descending colon were performed.
Immediate post-operative in ICU, after intensive therapies (sedative, muscle relaxant, mechanical ventilation, vasopressor support, fluid resuscitation and antibiotherapy treatment with meropenem and linezolid renal adjusted dose) hemodynamically stable, the patient was discharged from the ward on the 4th day of the re-intervention, presenting good oral tolerance, adequately preserved intestinal transit and normal abdominal exploration. Abdominal fluid culture came back positive for Klebsiella pneumoniae, Escherichia coli, Pseudomonas aeruginosa, and Candida albicans. Treatment was started with intravenous fluconazole 400 mg. every 12 hours; Linezolid was discontinued and we maintained the treatment with intravenous meropenem 2 g. every 8 hours and subcutaneous sodium bemiparin 2500 UI every 24 hours.
After 48 hours, the patient became unwell, suffering from significant asthenia, sleep tendency and hypotension, without neurological or abdominal focus, and serous drainage was preserved. It was associated with marked hyponatremia in the analysis without other significant findings (Blood tests: Sodium 119 mEq/L (normal range 136.0-145.0), Potassium 5 mEq/L (normal range 3.5-5.1)). Abdominal CT scan (Figure A) and basal cortisol in the blood were requested, compatible with bilateral adrenal hemorrhage and adrenal insufficiency (Blood tests: Cortisol 6.07 ug/dL (normal range 6.20-19.40)) with negative lupus anticoagulant and negative anticardiolipin antibody with normal thyroid function. Treatment with subcutaneous sodium bemiparin was discontinued and treatment with intravenous hydrocortisone 100 mg every 8 hours was initiated, with the recovery of blood pressure and natremia after the third day of treatment. (Blood tests: Creatinine 0.65 mg/dl (normal range, 0.0-1,20), Urea 47 mg/dL (normal range, 16-48), Sodium 137 mEq/L (normal range 136.0-145.0), Potassium 4.6 mEq/L (normal range, 3.5-5.1), White cell count x 109/L 13.9 x109/L (normal range 3.6-10.5) , Hemoglobin 8.4 g/dL (normal range 13.0-18.0), Hematocrit 24% (normal range 39.0-52.0), Coagulation: standard.
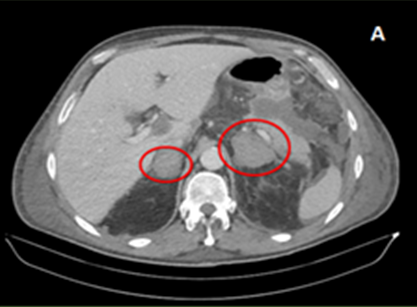
Figure A: Abdominal CT: Increase in size of both adrenal glands with an increase in homogeneous density of an average of 54 HU, hyperdensity, suggesting bilateral adrenal hemorrhage.
The intravenous corticoid was administered to the patient following a downward trend during two weeks (cortisolaemia 11.9 ug/dL (normal range 6.20-19.40) at hospital discharge. He presented favourable evolution, allowing the change to oral corticotherapy with hydroaltesone 20 mg every 12 hours. An abdominal CT scan at 15 days (Figure B) showed no further bleeding and some reduction in size of the adrenal glands with no other findings. Antibiotic treatment was completed taking 17 days’ time. The patient was discharged 21 days after re-operative abdominal surgery.
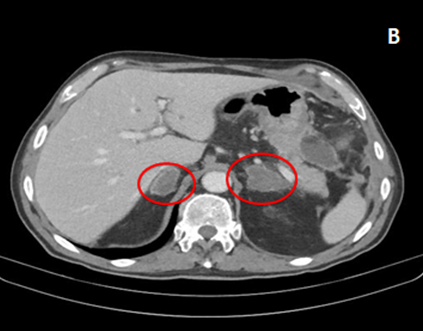
Figure B: Abdominal CT scan at 15 days: Decrease in the density of intraglandular contents with persistent focal areas of higher density indicating evolving bilateral adrenal hemorrhage.
The patient is currently asymptomatic, seven months after the surgical intervention, with normal blood pressure, without locoregional or distant recurrence (he received chemotherapy treatment for 6 months) and he is being monitored because of his residual chronic adrenal insufficiency, following treatment with hydroaltesone 5mg every 12 hours keeping standard levels of cortisol in blood.
Discussion
The adrenal glands are of intrinsic importance in the physiological response to stress, responsible for the maintenance of blood pressure and electrolyte homeostasis. In critically ill patients, unrecognised and untreated adrenal insufficiency is usually fatal and as the presentation of acute adrenal insufficiency is variable and non-specific, a high degree of clinical suspicion is required3.
Post-operative adrenal hemorrhage is uncommon and has fundamentally been reported in patients with previous risk factors: sepsis, heparin-induced thrombocytopenia, myocardial infarction, congestive heart failure and Anti-phospholipid Syndrome. However, it is more commonly associated with trauma, meningococcemia (Waterhouse–Friderichsen syndrome), and anticoagulation use2. Adrenal haemorrhage is most commonly seen in surgical patients in the first fourteen post-operative days1,2.
Standard diagnostic assessment is a non-contrast CT, which would demonstrate hyperdense adrenal enlargement2,3. It can present with fever, abdominal pain, obnubilation, weakness and hypotension, along with biochemical alterations such as hyponatremia, hyperkalaemia or hypoglycaemia1-3.
Our patient presented six days prior to the diagnosis of adrenal haemorrhage with peritonitis caused by multibacterial infection, in the context of a complicated post-operative period of colonic surgery (tumour pathology). In this sense, on the one hand, cancer cells affect the coagulation cascade and platelet activation to induce a prothrombotic state4. On the other hand, lipopolysaccharide is a mainstream constituent of the cell wall of gram-negative bacteria that can bind to endothelial and inflammatory cells as a highly potent activator, leading to increased transcription of proinflammatory cytokines and other mediators. In this way, sepsis (defined by a rise in Sepsis-related Organ Failure Assessment score ≥ 2 according to the working group´s SEPSIS 3)5 is associated with activation of procoagulant and fibrinolytic pathways and downregulation of anticoagulant pathways6. In addition, another factor that is thought to make the adrenal glands susceptible to haemorrhage is that the adrenal glands have a very rich arterial circulation that drains into a single central adrenal vein, causing at the microcirculation level a hypersensitivity to the hormones involved in the stress response (ACTH, catecholamines), causing an increase in blood flow over a vulnerable network, thus triggering an intraglandular hemorrhage2,3.
In this case, despite treatment for post-operative surgical complication with prompt re-operative abdominal surgery and intensive medical treatment, the patient presents with bilateral adrenal hemorrhage. Failure to promptly recognize and treat adrenal insufficiency after adrenal haemorrhage can be fatal. We consider this case interesting as it reveals the serious secondary consequences of a post-operative surgical complication. The rapid implementation of replacement therapy with hydrocortisone or methylprednisolone, after the determination of basal cortisol, together with the confirmation through CT, as in our case, is of great importance for the favourable evolution of the patient1-3. Although there are cases in which endocrine function is restored, most patients must receive cortisone replacement therapy indefinitely2,3.
Confidentiality of data
The authors declare that they have followed the protocols of their work center on the publication of patient data.
Conflict of interest
The authors declare no conflicts of interest of any nature.
References
- McNicol, RE et al. “Post-operative bilateral adrenal haemorrhage: A case report.” International journal of surgery case reports vol. 5,12 (2014): 1145-7. doi:10.1016/j.ijscr.2014.09.033
- Logaraj, Anthony et al. “Adrenal crisis secondary to bilateral adrenal haemorrhage after hemicolectomy.” Endocrinology, diabetes & metabolism case reports vol. 2016 (2016): 16-0048. doi:10.1530/EDM-16-0048
- Egan, Aoife M et al. “Bilateral adrenal haemorrhage secondary to intra-abdominal sepsis: a case report.” Cases journal vol. 2 6894. 9 Jun. 2009, doi:10.4076/1757-1626-2-6894
- Mitrugno, Annachiara et al. “The role of coagulation and platelets in colon cancer-associated thrombosis.” American journal of physiology. Cell physiology vol. 316,2 (2019): C264-C273. doi:10.1152/ajpcell.00367.2018
- Gül, Fethi et al. “Changing Definitions of Sepsis.” Turkish journal of anaesthesiology and reanimation vol. 45,3 (2017): 129-138. doi:10.5152/TJAR.2017.93753
- Guarner, Jeannette et al. “Adrenal gland hemorrhage in patients with fatal bacterial infections”. Mod Pathol.2008;21(9):1113-20.
